- 90% of individuals with MS develop urinary issues in <18yrs of their diagnosis
- Overtime, 80% of people with MS will experience some bladder issue
- 1 in 10 report bladder and urinary concerns at the onset of MS
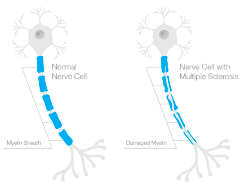
Multiple Sclerosis (MS) is an autoimmune neurological condition, where the body’s own immune system begins to attack nerve pathways within the brain and spinal cord. These ‘attacks’ produce slowing of conduction along the affected pathways over time. The attacks produce lesions (areas of damage) which are typically separated by time and space, thus, producing different types of clinical presentations over the course of the condition. The variable distribution of these lesions gives the condition its name, multiple (many) sclerosis (lesions).
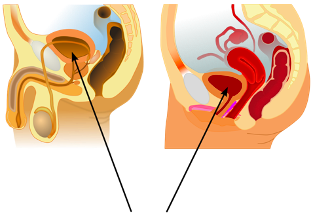
A common underdiagnosed and insufficiently treated symptom of MS is bladder dysfunction. The storage and excretion of urine from the bladder is a complex neurological mechanism. Individuals with MS with bladder filling or voiding difficulties frequently complain of the following:
- urinary urgency (a strong urge to use the bathroom)
- increased urinary frequency (frequent visits to the bathroom)
- increased urinary frequency during the night
- hesitation to void
- difficulty initiating a urine stream or a weak stream
- incomplete voiding, urinary retention in the bladder
- leakage of urine (incontinence)
The number of urinary complaints rise as the lesions in brain and spinal cord increase. Individuals with MS can have multiple urinary symptoms present during the course of their condition, therefore, requiring necessary reassessments and change of therapies.
Reasons for this variable presentation in MS could be due to a variety of causative factors, frequently determined by a urodynamic evaluation. Common causes include overactivity of the bladder muscle (seen in 53% of individuals) or an incoordination between the bladder muscle and the conscious urinary sphincter muscle during the process of voiding or urination (seen in 43% of individuals).
Primary lines of treatment for improving bladder function include medications which can reduce the overactivity of either bladder or sphincter muscles, and the use of pelvic floor muscle training. Evidence suggests that pelvic rehabilitation training can reduce the number of episodes of urinary incontinence, quality of life, severity of irritative symptoms and night-time urination in people with MS. Both medications and pelvic rehabilitation interventions should be explored for improving bladder symptoms in MS. Secondary lines of treatment include insertion of catheter tubes to drain the bladder, and other medical or surgical options.
Since urination is an essential component of everyday life, the treatment options should always gear towards improving the individual’s quality of life and safety. Due to the variability of urinary symptoms seen in MS, a targeted multidisciplinary approach may be helpful in achieving both, better quality of life and safety for each individual.
Hope you enjoyed this article! Please read, comment & share!
Hina Garg
PT, MS, PhD
Board-certified neurological clinical specialist
References:
- Riccardo Bientinesi, Carlo Gandi, PierFrancesco Bassi. Managing Urological Disorders in Multiple Sclerosis Patients: A Review of Available and Emerging Therapies. International Neurourology Journal. 2020;24(2):118-126. doi:10.5213/inj.2040028.014
- Pérez DC, Chao CW, Jiménez LL, Fernández IM, de la Llave Rincón AI. Pelvic floor muscle training adapted for urinary incontinence in multiple sclerosis: a randomized clinical trial. International Urogynecology Journal. 2020;31(2):267-275. doi:10.1007/s00192-019-03993-y
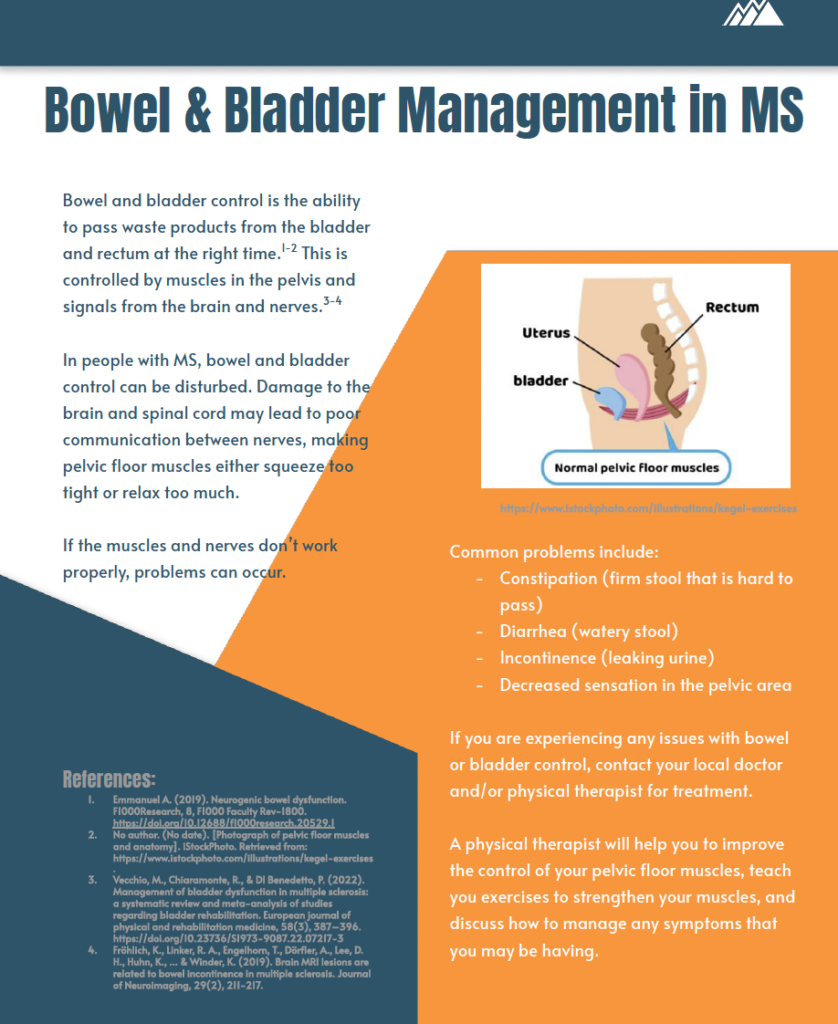
Here is a handout to explain the bladder and bowel function in people with MS. Share it with patients and providers to spread the word!
4,905 total views, 10 views today

Terrific article