< 5mins read
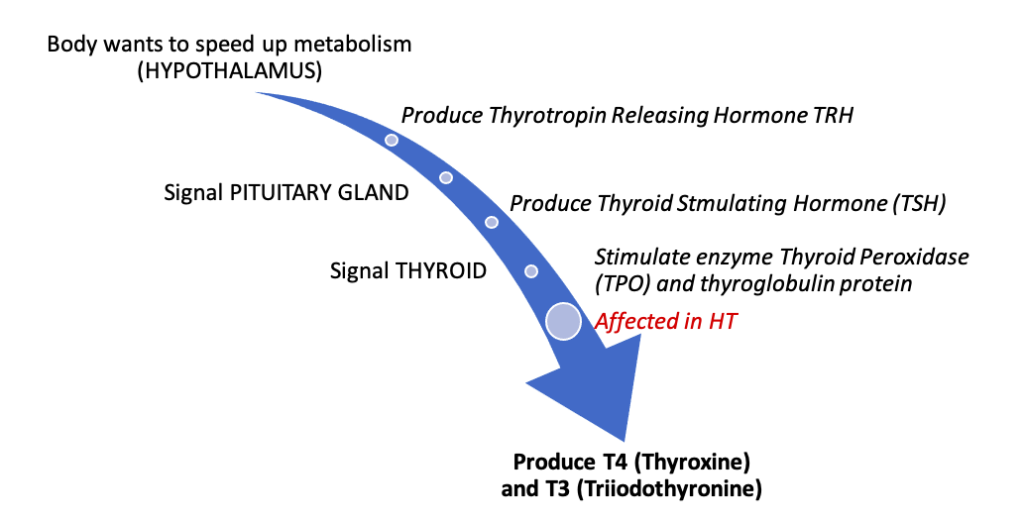
Hashimoto thyroiditis (HT) is one of the most common autoimmune conditions, where the body develops an immune response to two key thyroid hormone producing agents including the Thyroid Peroxidase (TPO) and thyroglobulin (see Figure below). The self-immune attack can result in lymphocytic infiltration, destruction and scarring of the thyroid tissue and create high levels of autoantibodies to the 2 key agents (TPO and thyroglobulin). HT typically affects women, between the ages of 30–60 years and is a growing diagnosis in Caucasians (5%), where it can present clinically with symptoms or remain subclinical (undiagnosed).
Normal physiology of thyroid and related hormones
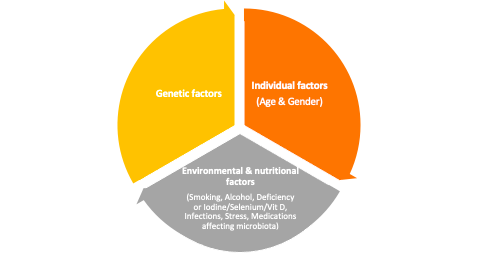
Common causes of HT: HT is considered to be associated with a complex mix of genetic, individual and environmental factors.
Symptoms of HT are typically not acute or specific. Some examples include:
- change in mood
- depression
- concentration problems
- brain fog
- biological changes: dry skin, hair loss, constant fatigue (even after good sleep), changes in body weight, disturbances in bowel movements
Behavioral management of HT
- Reduce immune triggers by following an Elimination Diet.
- Elimination or minimizing GLUTEN: The gliadin portion of gluten typically simulates the molecular structure of thyroid gland and, therefore, evokes an immune reaction. Gluten can become a trigger when found in blood instead of the intestines due to a “leaky gut”.
- Elimination of dairy products containing lactose.
- Elimination diets have been found to significantly reduce the autoantibodies to both TPO and thyroglobulin, and increase vit D in people with HT.
- Create a Nutrition Plan to support general thyroid health.
- Consume 4-5 meals matched to your energy requirements daily, including high fiber, plant-based fats, whole grain carbohydrates and 15-20% protein. See Table for specific recommendations.
- Include Essential Fatty Acids (EFAs) for healthy hormone production. Commonly found in cold-water fish, flax and chia seeds, evening primrose oil, borage oil, black currant seed oil, and in many raw, unprocessed nuts and seeds
- Eliminate refined sugar, trans fatty acids, artificial sweeteners, avoid overstimulation via caffeine
- Include organic foods, plenty of vegetables and water.
- A recent study determined that individuals with HT, as compared to general populations, typically consumed high levels of animal fat, processed meat and nuts, and low levels of red meat, plant or olive oil, and fruits (Kalicanin 2016). This suggests the need to execute a well-balanced nutrition plan in HT.
| Vitamin D | Fatty fish, fish oil, sun-dried mushrooms, Agaricus (and solar bath), chicken eggs |
| B group vitamins | Meat, fish, chicken eggs, wholegrain cereal products |
| Vitamin A | Kale, carrot, pumpkin, liver, spinach, egg yolk, butter, dried apricot |
| Vitamin C | Black currant, kiwi, strawberry, orange, mango, lemon, melon, kale, spinach, tomatoes, peppers (especially red peppers), vegetables and fruit |
| Vitamin E | Avocado, fish oil, whole-grain cereal products, vegetable oils |
| Magnesium | Cocoa and bitter chocolate, pumpkin seeds, avocado, nuts, whole grain cereal products, some fatty fish (salmon) and green vegetables, yogurt, kefir |
| Zinc | Cocoa and bitter chocolate, meat, kefir, yogurt, pumpkin seeds, nuts, spinach, mushrooms, whole-grain cereals |
| Iron | Meat, animal offal, cocoa and bitter chocolate, spinach, sardines, seafood, pumpkin seeds |
| Iodine | Iodized salt, fish (cod, tuna), seafood, seaweed, iodized milk and dairy products if elimination is not required, chicken eggs, plum, maize |
| Selenium | Brazilian walnut, fish (sardines, halibut, salmon, tuna), meat, spinach, liver |
- Reduce Stress.
- Stress upsets immune regulation by suppressing immune function, promoting immune imbalances, weakening the thymus gland, and thinning the barriers of gut, lungs, and brain
HT disease and its course can be significantly influenced by the nutritional, environmental and lifestyle factors in a person predisposed due to genetics and age or gender. Poor diet and lifestyle can affect the immune system’s activity, lose immune tolerance and develop autoimmune processes, therefore, highlighting the need for their consideration in effective patient management. Due to its autoimmune nature and the dietary associations, HT management should include additional screening to identify the co-occurrence of other diseases such as coeliac disease and inflammatory bowel diseases.
Hope you enjoyed the blog! Since most autoimmune and chronic conditions require behavioral modifications, consider sharing this information with your patients.
Hina Garg, PT, MS, PhD, CEEAA
Like, share or comment here…
References:
Paulina Ihnatowicz, Małgorzata Drywień, Paweł Wątor, Joanna Wojsiat. The importance of nutritional factors and dietary management of Hashimoto’s thyroiditis. Annals of Agricultural and Environmental Medicine. 2020;27(2):184-193.
Christine L. Sonchar. Medications alone are not the answer for an optimally functioning thyroid, instead healthy nutrition & lifestyle choices are the keys! Nutritional Perspectives: Journal of the Council on Nutrition of the American Chiropractic Association. 2016, 39(4): 11-13.
Dean Kaličanin, Luka Brčić, Katija Ljubetić, et al. Differences in food consumption between patients with Hashimoto’s thyroiditis and healthy individuals. Scientific Reports. 2020;10(1):1-10.
12,170 total views, 9 views today

Wow, this articlle is nice, my sister is analyzing such things, so I amm goinbg
to inform her.